GENERAL MEDICINE CASE DISCUSSION
68 years old lady with lower abdomen pain & Type II Diabetes
May 14, 2023
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box is welcome."I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan .
Cheif complaints :
68years old lady who is a resident of nalgonda came with
C/o loose stools 3-4 episodes per day since 1week
C/o pain abdomen since 4days
C/o fever with chills since 4days
C/o vomitings since 3days
C/o abdominal distension since 3days
C/o constipation since 2days
History of presenting illness :
Patient was apparently asymptomatic 1week back then she had c/o loose stools 3-4 episodes per day which lasted for 2days, watery, not a/w blood &mucus ,black coloured ,large volume followed by she had c/o pain abdomen in epigastrc region f/b diffuse colicky type(squeezing) & she also had c/o fever a/w chills which was high grde,intermittent, no evening rise of temperature, a/w vomitings, non bilious, non projectile ,food as content &abdominal distension. She also has c/o constipation since 2days.
Past History :
No history of similar complaints in the past.
K/c/o DM since 10 years on regular medication.
N/k/c/o HTN, Asthma, TB,CVD, CAD, Epilepsy
No past surgical history
No h/o blood transfusions.
Personal History :
Diet -Mixed
Appetite -Normal
Bowel & Bladder -Regular
Sleep -Adequate
No addictions & allergies
Family History :
Not significant
General Examination :
Patient is conscious,coherent, co-operative
thin built &moderately nourished
Pallor-absent
Icterus-Absent
Cynosis-Absent
Clubbing-Absent
Lymphadenopathy -Absent
Vitals @admission
Temp - 98.8F
PR- 116BPM
RR-22CPM
Bp-130/70mmHg
Spo2- 97%
GRBS-221mg/dl.
Systemic Examination
I) Per Abdomen :
INSPECTION :-
Shape of abdomen -Distended
Umbilicus - inverted
No scars, sinuses, straie
No visible pulsations & visible peristalsis
Movements of all 4 quadrants moving equally with respiration
PALPATION :-
All inspectory findings are confirmed
No local rise of temperature
Tenderness present in the epigastric region
No palpable mass present
No palpable lymphadenopathy
No organomegaly
Hernial orificies - Free
PERCUSSION :-
No signs of fluid thrill & shifting dullness
Resonant note heard (except liver dullness)
AUSCULTATION :-
Bowel sounds present
II) Respiratory system :
Normal vesicular breath sounds heard
Bilateral air entry present
No added sounds
III) CVS:-
S1S2 heard ,No murmurs
IV) CNS :-
NAD, HMF intact
Investigations :-
15/5/23
Hemogram
CUE
15/5/23
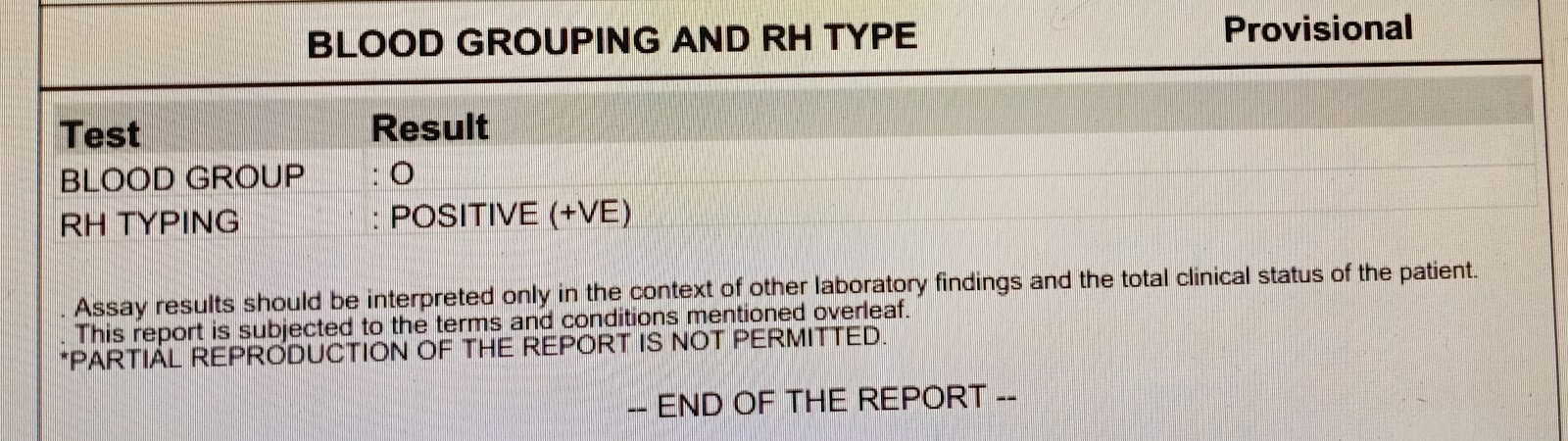
Blood group - O positive
Malarial parasites - Negative
ESR - 8 mm/1st hour
PT - 15sec
INR -1.11
Aptt -31 sec
Reticulocyte count - 0.5%
RBS- 230mg/dl
LDH - 258 IU/L
RFT :-
Blood urea-52mg/dl
sr.creatinine- 2.4 mg/dl
Sodium -135mEq/L
Potassium - 4.1mEq/L
Calcium - 1.06mmol/L
Chloride- 101 mEq/L
Sr.Magnesium - 2mg/dl
LFT :-
TB - 1.37 mg/dl
DB- 0.26mg/dl
AST - 16IU/L
ALP - 15 IU/L
ALP - 497 IU/L
TP - 5.5gm/dl
Albumin - 2.6gm/dl
A/G ratio - 0.92
Serology - Negative
C-reactive protein - positive
16/5/23
Hb - 9.9 gm/dl
TLC - 15,600 cells/cumm
N/L/E/M - 83/10/1/6
PLT - 1.50
16/5/23
RFT :-
Blood urea- 63mg/dl
sr.creatinine- 2.7mg/dl
Sodium -135mEq/L
Potassium - 3.9mEq/L
Calcium - 1.06mmol/L
Chloride- 98mEq/L
17/5/23
Hb - 10.6gm/dl
TLC - 13,700 cells/cumm
N/L/E/M - 70/18/1l2/10
PLT - 1.56
16/5/23
RFT :-
Blood urea- 75mg/dl
sr.creatinine- 2.7mg/dl
Sodium -135mEq/L
Potassium - 4mEq/L
Calcium - 1.06mmol/L
Chloride- 103mEq/L
Urine for ketone bodies - negative
X-ray erect abdomen
ECG
2decho